Eating Disorder Awareness Week: 24 February – 2 March 2025
Eating Disorder Awareness Week: 24 February – 2 March 2025
Reader’s Digest: An insight into eating disorders
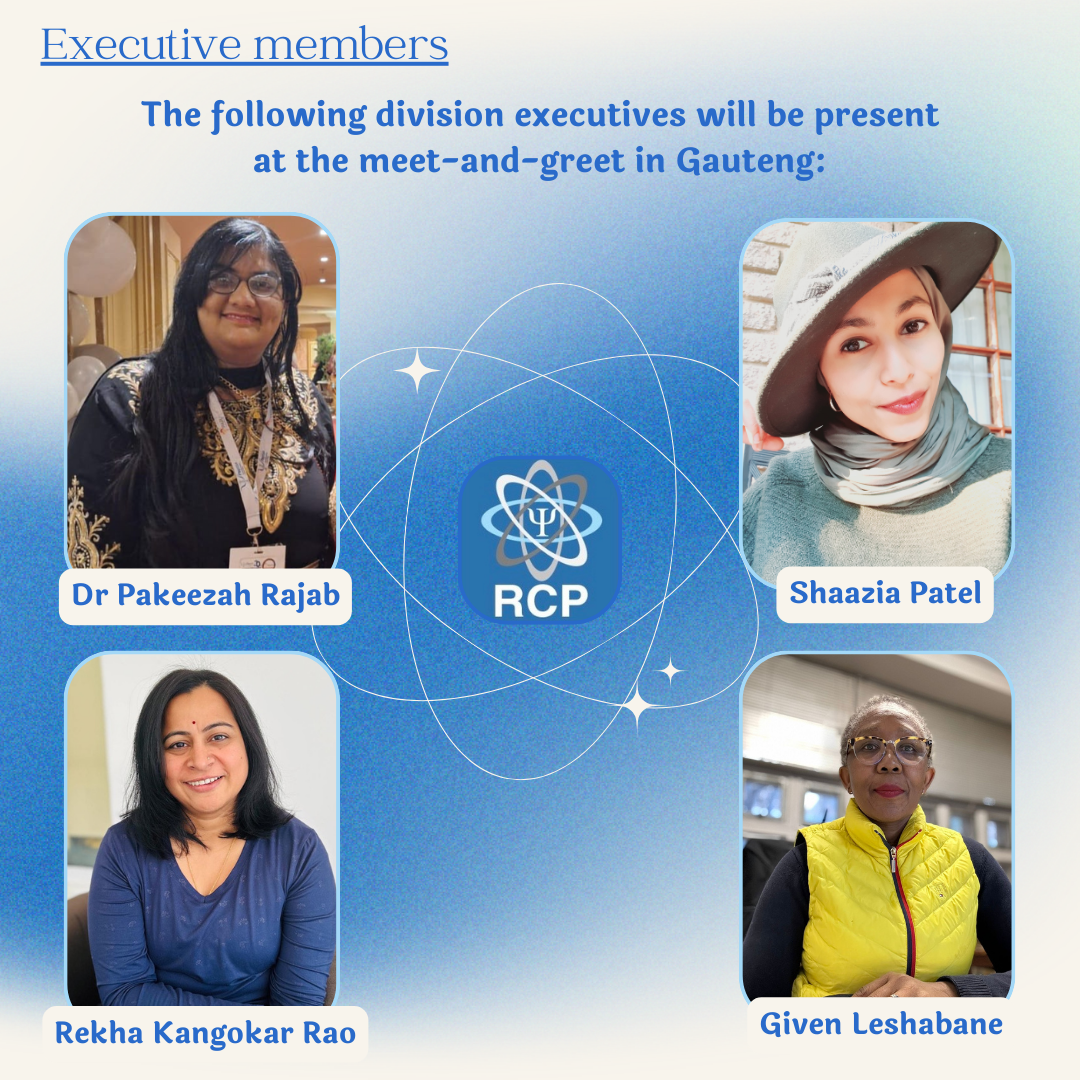
Authors: Z. Hoosen, G. Burrow, R. Kangokar Rama Rao (The Registered Counsellors and Psychometrists’ Executive Committee)
The frequency of eating disorders has almost doubled globally in less than 20 years and continues to rise (Center for Women’s Health, N.D.). The American Psychological Association defines an eating disorder (ED) as “any disorder characterized primarily by a pathological disturbance or attitude and behaviours related to food” (APA, 2018). The ICD-10 classifies eating disorders into two principal syndromes: anorexia nervosa and bulimia nervosa. Furthermore, binge eating disorder is also classified with this spectrum of disorders.
The Eating Disorders South Africa organisation briefly describes that anorexia and bulimia nervosa are commonly associated with the following behaviours: adherence to strict diets despite weight gain/loss, compulsive exercising for weight loss, binge eating large quantities of food, consuming laxatives or diuretics aimed at purging or expelling food intake, abuse of stimulants or similar substances such as appetite suppressants etc. More definitively, the National Institute of Mental Health (NIMH) indicates that anorexia nervosa is characterised by a significant and persistent reduction in food intake resulting in low body weight in the context of age, sex, and physical health; an unrelenting pursuit of thinness; distorted body image and intense fear of weight gain, and severely disturbed eating behaviour (NIMH). Then, bulimia nervosa is characterised by bingeing (eating large amounts of food in a short period, often accompanied by a loss of control) followed by behaviour that compensates for the binge, such as purging (e.g. vomiting, excessive use of laxatives, or diuretics), fasting, and/or exercise. A common distinctive feature between anorexia and bulimia is that individuals suffering with bulimia can fall within the normal range for their weight. However, individuals suffering from anorexia often display a deep fear of gaining weight, desperately want to lose weight and experience persistent dissatisfaction with their body size and shape (NIMH).
The global burden of disease study found a significant burden of eating disorders (EDs), specifically among young women living in high-income countries (Williams et al., 2020). Correspondingly, Markino et al. (2004) had previously found that more females suffered from EDs and displayed abnormal eating attitudes than males in at least 11 countries. In contrast, Novotney (2024) argue that boys and men are increasingly becoming affected by mental health conditions such as body dysmorphia and subclinical disordered eating behaviours. It is reported that males now constitute approximately a third of those diagnosed with an eating disorder (Mitchison, 2019), highlighting a growing concern around this clinical concern.
Further, it was found that the prevalence of EDs in non-Western countries was lower than Western countries, although this has since gradually increased (Markino et al., 2020). Evidence suggests that gender and sociocultural influences play a role in this increase (Hoek, 2016; Markino et al., 2020). Commonly, the attitudes, social influences, and media depictions of physical features of ‘perfection’ such as ideal thinness or ideal muscularity are strongly cited as risk factors for both males and females. Unfortunately, the median onset of EDs is in the late teens to early 20s (Kessler et al., 2013; Glazer et al., 2021).
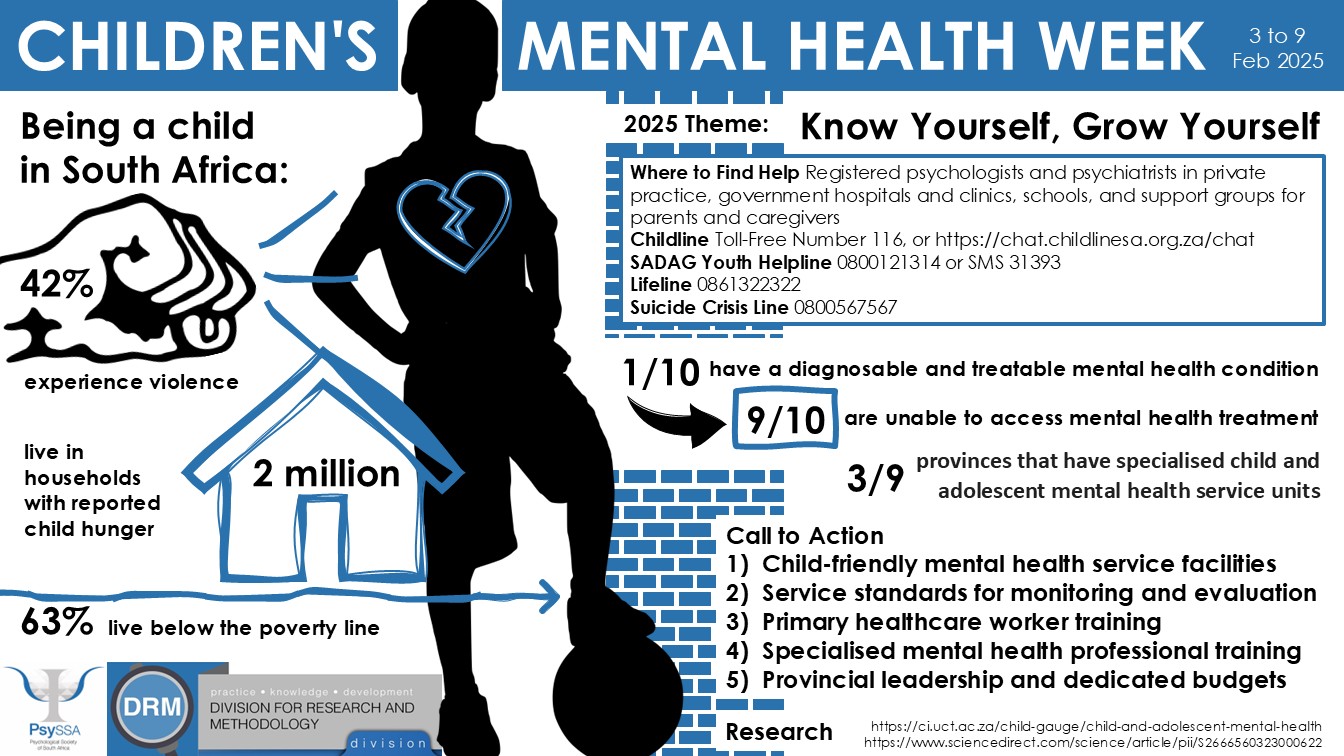
Eating disorders are complex mental health conditions that often manifest during adolescence, typically between the ages of 12 and 25. Common types include anorexia nervosa, bulimia nervosa, and binge eating disorder. A combination of genetic, psychological, and sociocultural factors influences the onset of these disorders. Early intervention is crucial, as timely treatment can significantly improve recovery outcomes. Parents, educators, and healthcare professionals should be vigilant for warning signs, such as drastic weight changes, preoccupation with food or body image, and avoidance of meals. Promoting a healthy relationship with food and body image during these formative years is essential for prevention and early detection (Tan et al., 2022).
Treatment and support
A crucial aspect of treating EDs is detecting disorders as early as possible. Reports from practitioners highlight that being more aware of body image and eating concerns is an important part of the treatment process (Novotney, 2024).
Ideally, treatment for EDs involves a multidisciplinary approach, often including a range of licensed and qualified professionals, including a medical practitioner, a mental health professional such as a psychiatrist or a psychologist, a nutritionist, and/or a dietitian. These professionals are identified as trained and educated to provide a holistic treatment for an individual that treats affected areas of functioning and equips the individual with the necessary intervention to recover.
An infographic of a treatment intervention is attached to this article for educational purposes. The aim of this infographic is to provide practitioners such as registered counsellors with an insight into a treatment plan that may be applied to a case where an individual suffers from an eating disorder. The summary formulation presented below is for educational purposes and highlights key aspects common in cases of eating disorders. This article and its contents do not serve as a medical or professional mental health opinion or diagnosis. If you or anyone you know might be experiencing any of the points below, we strongly urge you to reach out for support via the helplines and contact centres found at the end of this article.
Role of the registered counsellor
A registered counsellor (RC) in South Africa plays a vital role in early intervention, psychoeducation, and brief therapeutic support for clients with eating disorders (EDs). While RCs do not diagnose or provide long-term psychotherapy, they can provide preventative care, short-term interventions, and referrals to psychologists, dietitians, and medical professionals.
Eating disorders in South Africa are often underreported due to cultural stigma, lack of awareness, and limited access to specialist services. The RC’s role is to create awareness, offer psychoeducation, and provide short-term intervention using evidence-based techniques like Cognitive-Behavioural Therapy (CBT), psychoeducation, and strengths-based approaches.
Please refer to the infographic attached for the example treatment plan.
Support services and organisations:
- RecoverySpace.org focuses on promoting recovery from eating disorders. The site provides information on various eating disorders, as well as treatment options and recovery tools & tips. The organization provides support to individuals currently in recovery, and includes coaching (via e-mail and online sessions), as well as regular webinars.
Email: info@recoveryspace.org
- Eating Disorders South Africa (EDSA) renders a variety of eating disorder treatment services including both in and out-patient services as well as aftercare for eating disorders. More information can be found at edsa.co.za.