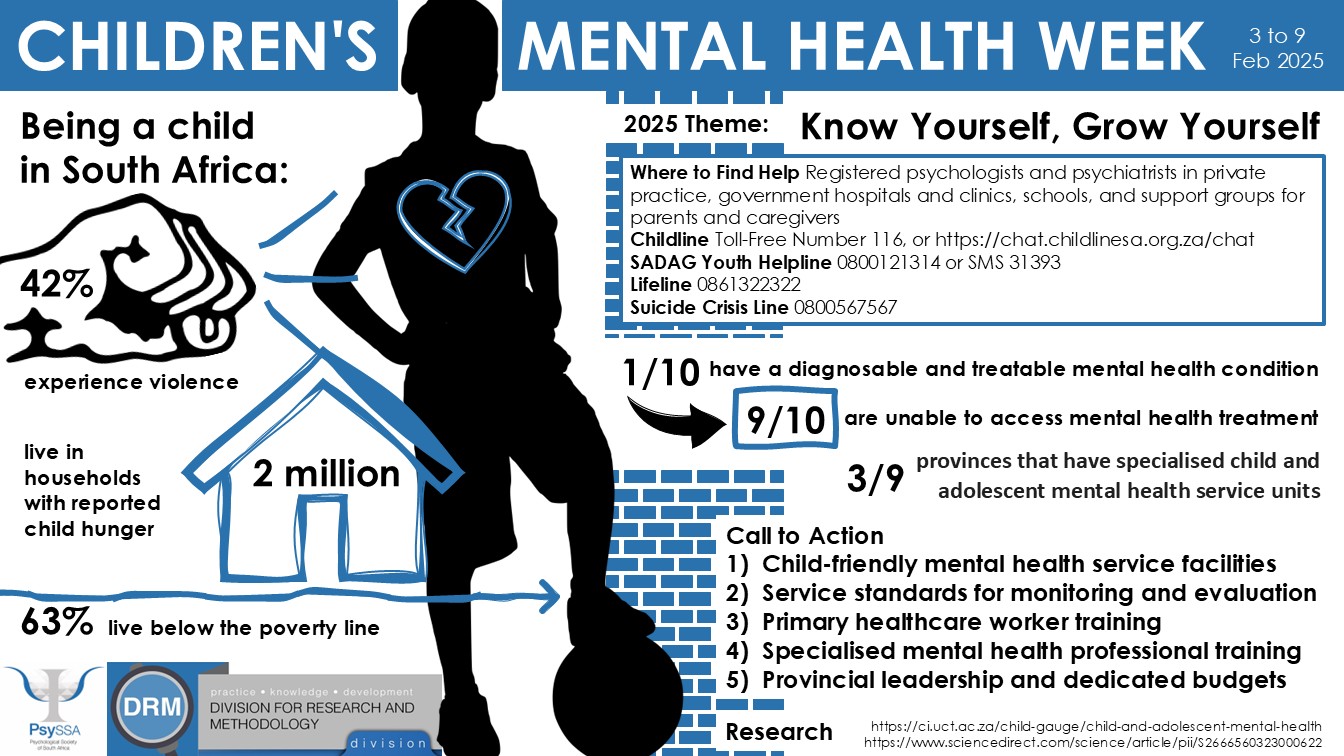
Children’s Mental Health Week: 3-9 February 2025
PsySSA commemorates Children’s Mental Health Week (3-9 February 2025) with the theme: Know Yourself, Grow Yourself.
CHILDREN”S MENTAL HEALTH WEEK: 2025
PSYSSA is complimented for launching the 2025 MHC with the focus on Children’s Mental Health. Children have a special place in Society. They are the archetypal pride and joy of parents associated with fun, laughter, joy and playfully mischievous in a normal society. Parents generally promote their healthy living through social, emotional, psychological, and spiritual well-being. The seminal Children’s Act 38 of 2005 and amendments profoundly spell out how children must be cared for and protected.
While there were adverse conditions prior to the drafting of the above Act, the current children’s mental health needs have reached uncontrollable proportions. This in fact has given rise to grave concerns for their mental health and fears for their safety. It would make for un-sobering reading to take a snapshot view of how children are faring with their Mental Health globally. Space does not allow for such a broadside perspective. WHO (2022) presents the startling statistic that twenty five (25%) of children present with Mental Health issues. A UNICEF South African Report posited that sixty (60%) of youth needed mental health support. However, only 12.4 % of children and adolescents with mental health problems receive professional help (Kleintjies et al., 2015). This can be explained by the gross imbalance between psychologists and patients. According to the SAACP ( 2020) there were (3022)-Clinical Psychologists; (1598)-Counselling Psychologists: (1510).-Educational Psychologists.
This translates to a ratio of about 1 psychologist for 10 633 clients. At a systemic level this overwhelming inequity explains why children in general find it difficult to access Mental Health services. This situation is further exacerbated by the fact that the majority of the practitioners are in private practice. This begs the question what if any mental health intervention children from the rural area receive. The psychological services attached to the various districts in each province can hardly be considered to be a serious service provider of mental health. Statistics from eight DOE provinces (2020-2021) underscore the stark and gloomy reality of the effete mental health school provisions :
| Province | Pupils | Psychologists |
| Eastern Cape | 1 704 581 | Unknown |
| Free State | 541 959 | 15-20 |
| Kwa Zulu Natal | 2 758 831 | 83 |
| Limpopo | 1 245 095 | 30-35 |
| Mpumalanga | 745 838 | 25 |
| North West | 584 831 | 20-25 |
| Northern Cape | 272 411 | 15-20 |
| Western Cape | 1048 905 | 47 |
| Gauteng | 2 055 042 | 45 |
An overpowering disproportion between pupils and psychologists. It is noted that formal assessments cannot be administered for this reason. In any case it is apparent that psychologists only respond to a request from a school about twelve months later However, the inordinate disparity in numbers make access to mental health impossible for the majority of pupils. To a large extent detractors to the existence of school psychology are justified. It is an expensive service. It is a first world phenomenon in an under-developed third-world context.
The general public is hardly and selectively serviced, schools are poorly-serviced and the rural areas are abysmally non-serviced. Are we paying attention to the scary Big Picture or merely going through the motions like school psychological services. As the mental needs of our children get more complex and demanding are we psychologists playing the proverbial fiddle. Severe trauma, depression, anxiety, stress and suicide ideation are major psychological constructs that children experience. Their mental health needs are utterly under-provided. In the recent Mental State of the World Report released by Sapiens Labs South Africa ranked
Second(2nd) Lowest on the Mental Health Quotient
First as the most stressed country in the world
A recent advert notes that the “ difference is in the detail ”. We are patently aware of the appalling details. We need to step out of the comfort zones in our insulated ivory towers and make the difference.

Children’s Mental Health Week – Reflections on Self-Awareness as a Psychology Student
Children’s Mental Health Week, established in 2015, focuses on raising awareness of children’s mental health and emotional well-being. While this initiative originates in the UK, it aligns with local efforts such as Child Protection Week, Youth Month, and Mental Health Awareness Month, which highlight mental health challenges in childhood and beyond. This year’s theme, “Know Yourself, Grow Yourself,” provides an opportunity for psychology students to reflect on their own childhood mental health, exploring how their experiences have shaped their self-awareness and career paths.
Reflecting on childhood mental health often reveals how early challenges, trauma, or environmental factors influenced our mental well-being and led us to pursue psychology. Such reflections form the foundation of self-awareness, which is important for professional practice. Many psychologists embody the concept of the wounded healer, where their own struggles and healing journeys inspire their ability to empathise with others. Self-awareness allows individuals to recognise and work through biases, blind spots, and unresolved issues. For this reason, postgraduate applications, such as honours and master’s programmes, often include reflective exercises like autobiographical essays or interviews. These assessments evaluate not only academic readiness but also insight into one’s personal growth.
Self-awareness is not a one-time exercise but a lifelong process. As students, individuals continuously uncover values, insecurities, and unresolved emotions that shape how they engage with others. Discoveries like these follow practitioners into their careers, where self-reflection and professional counseling are essential for managing personal challenges and ensuring that mental health does not negatively impact those they serve. Early mental health struggles, such as emotional stressors or disorders, may persist in different forms, but when approached with self-awareness, they become tools for empathy and professional insight.
Across psychology’s diverse fields, self-awareness is critical in varying ways. Clinical and counselling psychologists rely on this quality to manage transference, countertransference, and emotional regulation, ensuring effective care without compassion fatigue or burnout. Educational psychologists use self-awareness to recognise how their own experiences and biases influence their work with children, families, and educators, enabling culturally sensitive interventions. Research psychologists depend on reflexivity to remain ethical and objective, particularly when working with vulnerable populations. In neuropsychology, awareness of one’s emotional responses helps practitioners manage the toll of working with life-changing diagnoses, balancing empathy with clarity. For organisational psychologists, self-awareness supports the management of workplace dynamics, promoting systemic well-being and addressing burnout.
Children’s Mental Health Week encourages us to reflect on our own mental health, using this theme as a starting point for cultivating self-awareness. This reflection reminds us that self-awareness is a lifelong journey, essential for both personal growth and professional competency. By engaging in self-awareness, we enhance our ability to empower the individuals and communities we serve.